A simple plan helps anyone working on medical device design. Both experts and beginners face problems. These problems include high costs, tough rules, and careful risk checks.
| Challenge Category | Example Issues |
| Development Costs | High R&D spending, clinical trials, special skills needed |
| Regulatory Complexity | Dealing with FDA, ISO 13485, IEC 60601, MDR rules |
| Manufacturing Challenges | Finding skilled partners, keeping quality, managing product life |
Using clear steps keeps things safe, good, and legal at each step.
Key Takeaways
- First, learn what users really need to make safe and good medical devices.
- Plan early for rules and risk control to stop expensive delays and keep things safe.
- Use clear design steps and write down details to help make the device, and follow the rules.
- Test early models often and listen to user feedback to make the device better before it gets approved.
- Keep checking devices after we are sold to fix issues and keep users safe for a long time.
User Needs
Knowing what users need is the first step in making a good medical device. Teams should find out what users really want. We should not just guess or make assumptions. This helps the device work well in real life.
Intended Use
Regulatory groups say intended use means the main reason for the device. It covers the health problem, who will use it, where it will be used, and what it does. Makers must write down the intended use in all files, labels, and ads. These documents must match each other. If we do not match, it can slow down approval and sales. Rules like ISO 13485 and FDA guides need full details, not just a short note. Intended use shapes the whole plan for rules and helps prove the device is safe and works well.
Stakeholder Input
Getting ideas from stakeholders early helps make better devices. Stakeholders are doctors, patients, business people, and rule experts. We can use many ways to get feedback:
- Surveys and focus groups show problems and needs.
- Watching people work helps us see what happens each day.
- Talking to users and testing shows what is hard or easy.
- Market research finds what is missing and what is needed.
A user-centered design uses all these ways to hear what users want. We share design ideas clearly and check if we can make them. Adding rules and market needs early makes things go faster. We must always think about risks and check for dangers at every step. Making and testing models helps us get feedback and make things better. Using human factors engineering makes sure devices are safe, easy to use, and work well for everyone.
Tip: Talking to real users, not just guessing, helps make safer devices, work better, and sell more.
Medical Device Classification
Knowing how to put a medical device into a group is important. This step helps the whole process go smoothly. Regulatory agencies use risk to sort devices. The FDA has three classes for devices. Class I is for low-risk things like tongue depressors. Class II is for medium-risk items such as catheters. Class III is for high-risk devices like coronary stents. Each class has its own rules to follow. Class I devices have general controls. Class II devices need general and special controls. Class III devices must get premarket approval. This system changes how fast a device can be sold.
Regulatory Pathways
Different places have their approval steps. The table below shows the main ways in the United States, Europe, and Asia:
| Region | Primary Regulatory Pathways / Programs | Key Features / Notes |
| United States | FDA 510(k), De novo, Premarket Approval (PMA), Breakthrough Devices Program | 510(k) for similar devices, De novo for new low/moderate risk, PMA for high risk, BDP for innovative devices |
| Europe | Medical Device Regulation (MDR), Health Technology Assessment Regulation (HTAR) | MDR harmonizes EU rules, HTAR focuses on clinical and cost-effectiveness, joint assessments start in 2026 |
| Asia | IMDRF, MDSAP | International harmonization, MDSAP allows single audits to be accepted by several countries |
Makers must pick the right path for their device. We should think about the class and what the market needs. Choosing early helps stop delays that cost money.
Early Planning
Planning for rules early stops problems later. We should start tracking rules from the start. With NOBLE’s reliable design and development expertise, we can confidently use special software and dashboards to monitor progress. We can use special software and dashboards to watch progress. Keeping good records, like Design History Files and Risk Management Files, helps track everything. By involving NOBLE’s professional technical team early, companies can identify and mitigate risks before they escalate. The FDA’s Innovation Pathway program shows that working with rule groups early can help get approval faster. We that set clear goals and agree on what data is needed do not waste time testing too much. Good planning makes sure the device is safe and works well. This helps the device get to market faster.

Design Controls
Design controls are very important for making safe products. The FDA and ISO 13485 say companies must use a clear process. With NOBLE’s proven design and manufacturing capabilities, this process is efficiently managed to ensure every medical device is safe and functions as intended. NOBLE’s experienced technical team supports clients at every stage—from initial planning through prototyping to final product verification. Their strong focus on quality and compliance ensures that design controls are followed precisely, reducing the risk of errors or costly recalls.
Documentation
Good documentation is needed to follow the rules and track changes. The FDA 21 CFR Part 820.30 and ISO 13485:2016 have rules for design controls. The table below shows how these rules match up:
| FDA 21 CFR Part 820.30 Design Control Element | ISO 13485:2016 Design and Development Clause |
| (a) General | 7.3.1 General |
| (b) Design and development planning | 7.3.2 Design and development planning |
| (c) Design input | 7.3.3 Design and development inputs |
| (d) Design output | 7.3.4 Design and development outputs |
| (e) Design review | 7.3.5 Design and development review |
| (f) Design verification | 7.3.6 Design and development verification |
| (g) Design validation | 7.3.7 Design and development validation |
| (h) Design transfer | 7.3.8 Design and development transfer |
| (i) Design changes | 7.3.9 Design and development changes |
| (j) Design History File | 7.3.10 Design and development files |
Each item in this table is a step that needs to be recorded. We record plans, inputs, outputs, reviews, checks, and changes, while also maintaining a design history file (DHF) containing all the details. This file is useful for audits and rule checks.
Note: If records are missing, approval can be slow or stopped. Without records, it is hard to show that a device is safe and meets all rules.
Good records help us track every choice and change. If something goes wrong, we can find and fix the problem fast. The Bjork-Shiley heart valve recall showed that bad records and weak design controls can hurt patients and cause trouble for companies. Good records keep patients and companies safe.
Risk Management
Risk management is a big part of design controls. ISO 14971 is the main rule for risk management in medical device work. The process has many steps:
- Risk Management Planning: We set the plan, goals, and tasks for risk work.
- Risk Analysis: We find dangers and guess how likely and bad they are.
- Risk Evaluation: We pick which risks need control using set rules.
- Risk Control: We pick and use ways like design changes, safety parts, or user lessons.
- Residual Risk Acceptability: We check if the leftover risks are okay.
- Risk Management Review: We look over all risk work and results.
- Production and Post-Production Monitoring: We watch risks after the device is sold.
Tip: Get people from engineering, quality, marketing, and users to help find all risks.
NOBLE integrates design controls and risk management as a unified process. Our thorough verification and validation testing ensure that risk controls are effective and reliable. This approach not only reduces the chance of errors and costly recalls but also supports full regulatory compliance—helping protect both patients and your reputation.
Design Inputs
Requirements
Design inputs are the main ideas for a medical device project. We must write these inputs carefully and clearly. Good design inputs help the device meet user needs and follow rules. They also help with checking and testing later.
Strong design inputs have these key parts:
- Use clear words so no one gets confused.
- Make sure each statement can be tested.
- Connect each input to the user’s needs and intended use.
- Cover all performance, rules, functions, and safety needs.
- Use ideas from standards, rules, old projects, other products, user feedback, and models.
- Have special people check and approve the inputs.
- Do not allow any confusing or mixed-up statements.
FDA rules say the manufacturer must write down how they make design inputs. These steps must talk about the intended use and user needs. ISO 13485:2016 says design inputs must include function, performance, safety, and rule needs. They must also use info from old designs and risk work. The manufacturer may spend up to 30% of the project time on this step. If inputs are not clear, big problems can happen after launch.
Risk Analysis
Risk analysis at this step helps us find dangers early. By looking for all possible failures, we can fix risks before we reach patients. Writing down why safety choices are made is very important. This helps keep the device safe and stops recalls.
| Example | Root Cause | Prevention via Risk Analysis at Design Input Stage |
| Inadequate User Need Translation | Design inputs missed user needs for material safety, causing skin irritation | Early risk checks, usability tests, and tracking between user needs, material details, and test plans |
| Missing Verification for a Key Output | Design changes not linked to updated verification steps, causing performance issues | Good change management, automatic links to tests, and updated records |
| Component Incompatibility Discovered Too Late | Firmware and hardware were not coordinated, leading to a device recall | Team reviews, working together, and better control of changes |
Doing risk analysis now helps us fix dangers before they get worse. This makes everyone trust that the device is safe and works well. With NOBLE’s expert technical support and deep experience in risk management, we can identify and address problems proactively.
Concept and Feasibility
Concept Development
Concept development is when we turn user needs into ideas. With NOBLE’s strong design and prototyping capabilities, we can explore a wide range of concepts through sketches and early models. Early on, we make simple models or pictures. These help everyone see how the device could work.
Most medical device ideas do not make it past this step. Many of us fail early in development. About 90% of medical technology ideas fail at the first test. The table below shows why many ideas do not move forward:
| Reason for Failure | Description |
| Unmet user needs | The device does not fix real problems, or is hard to use |
| Lack of expertise | We do not have the right skills or rule knowledge |
| Regulatory issues | We do not plan well for approvals and rules |
| Limited resources | We do not have enough people or money |
| Poor communication | We do not share information |
We ask experts from engineering, clinical, and rule fields to help. We also check if their ideas match what users want before going on. By partnering with NOBLE, we gain access to expert support across engineering, clinical, and regulatory fields. NOBLE’s collaborative approach ensures that every idea is evaluated not only for technical feasibility but also for user relevance. This alignment with real-world needs—early in the process—helps avoid costly missteps and sets the stage for a successful product launch.
Feasibility Study
A feasibility study checks if the idea can work in real life. NOBLE uses different ways to test if the idea is possible. Some ways are:
- Talking to users to see if the idea helps them.
- Doing small tests to see if the device works.
- Using studies to look at what could happen.
- Mixing numbers and user thoughts for a full view.
- Testing how to collect data and use the device to find problems.
NOBLE looks for signs that the device is safe and manufacturable, and we also check whether the resources needed for manufacturing are available. About 75% of medical device startups in the US fail, often because we skip this step. Careful studies help us avoid big mistakes and do better.

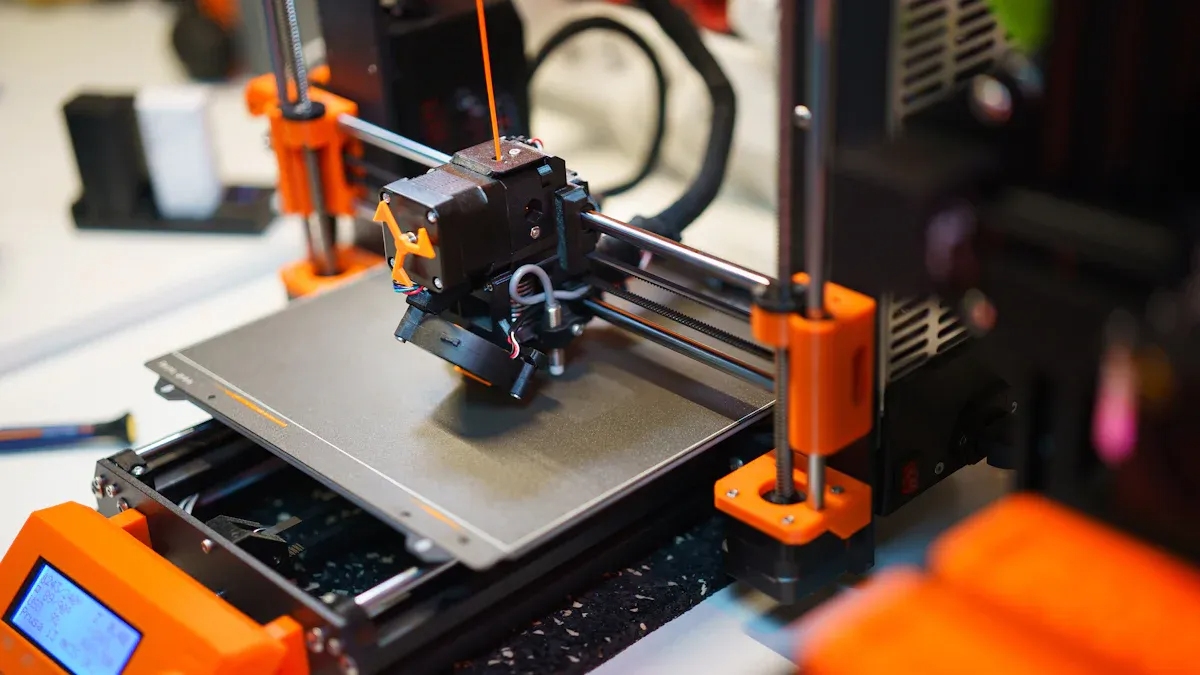
Medical Device Prototyping
Iterative Testing
Prototyping gives us a way to turn ideas into real, tangible devices. At NOBLE, we specialize in building early versions of medical products that can be tested in real-world settings. Through close collaboration with healthcare professionals and end users, we gather valuable feedback to identify what works—and what needs improvement. This process, known as iterative testing, is a key part of NOBLE’s development approach, ensuring that each prototype moves closer to a safe, effective, and user-friendly final product.
During each development cycle, engineers and designers at NOBLE make targeted improvements based on real-world test results. We might adjust the shape, size, or materials to enhance comfort, usability, or performance. For example, if a device feels too heavy, NOBLE’s team can quickly explore and prototype lighter material options in the next version. Healthcare professionals test these updates in controlled environments to ensure the device is easy to use, safe, and durable for everyday clinical use.
NOBLE’s iterative prototyping process is designed to identify and resolve issues early—well before the product reaches the market. This not only saves time and development costs but also ensures the device aligns with safety regulations and quality standards. Each round of feedback and refinement brings the design closer to meeting real user needs. With every cycle, NOBLE helps move the product toward a final version that performs reliably and meets all project goals.
User Feedback
User feedback is a key part of making a good medical device. We need a clear plan to collect and use feedback during prototyping. We start by setting goals for feedback and choosing the right users to test the device. We decide when and how to ask for feedback, such as through interviews, surveys, or hands-on trials.
Best practices for collecting and using feedback include:
- Define feedback goals and target users.
- Pick feedback methods that fit the device and users.
- Organize and study the feedback to find patterns.
- Use the feedback to make design changes.
- Check if the changes improve the device and adjust the process as needed.
We use tools to track and study feedback. We look for ways to make the device safer, easier to use, and more effective. By listening to users, we can spot problems that might not show up in lab tests. This process helps create a device that works well in real life and meets user needs.
Verification and Validation
Design Verification
Design verification checks if the device matches what was planned. We use this step to make sure the device works right before moving on.
Some important things for design verification are:
- We need to write down the steps for checking.
- We do tests, look at the device, and use models.
- All results must be written in reports and records.
- If there are problems, we fix them and check again.
At NOBLE, the main goal is to ensure every device matches the original design plan and performs safely and effectively. If any issues are found, our expert team quickly makes the necessary design changes and retests to confirm improvements. This proactive approach helps prevent costly delays, product recalls, and regulatory setbacks—keeping development on track and ensuring a smooth path to market.
Design Validation
Design validation at NOBLE confirms that the device works as intended for real users in real-life situations. We conduct thorough testing using actual or near-final prototypes to ensure the product is safe, effective, and ready for market.
Steps in design validation often are:
- Make a clear plan and give people jobs.
- Write down what users need and how the device will be used.
- Set clear goals and ways to check if the device passes.
- Review the design with experts from different areas.
- Test the device in real or fake situations.
- Test if real users can use the device easily.
- Check for risks and test software if needed.
- Write all results in the Design History File (DHF).
- Review and agree on any changes to the design.
- Make sure the design is ready to be made.
Validation can include clinical trials, checking packages, and looking at labels. We must show the device works for its users. We keep all records so we can be checked later.

Medical Device Manufacturing
Quality Controls
Quality controls are essential for making safe and reliable medical devices. At NOBLE, we follow strict standards like ISO 13485 to guide every step of our work. Using advanced tools, computer modeling, and simulations, we identify potential issues early—long before production begins.
Our smart manufacturing systems—powered by precise machinery and automation—help us deliver faster, more consistent results. NOBLE’s team receives ongoing training to stay current with the latest quality standards and regulatory updates.
We follow a disciplined process at every stage of device development. This includes thorough testing for function, durability, safety, environmental resistance, and cleanability. At NOBLE, cross-functional experts review each design to catch problems early and reduce risk before full-scale production.
Our robust Quality Management System (QMS) oversees every phase—from design to delivery—ensuring full traceability and compliance. Through regular audits and proactive risk management, NOBLE maintains the highest standards. Working with an ISO 13485–certified manufacturer like NOBLE builds trust, protects patients, and ensures lasting product success.
Supplier Management
Supplier management is important for making good and safe devices. Companies must make sure suppliers follow rules and industry standards. Rules like FDA 21 CFR 820.50 and ISO 13485:2016 Section 7.4 say companies must check and watch their suppliers. NOBLE uses modern Quality Management System (QMS) software to track supplier performance, compliance, and potential risks in real time. This proactive approach helps us identify issues early, avoid delays, and ensure that only high-quality components are used in every device.
Modern QMS software helps companies watch suppliers better. It checks how well suppliers do, if we follow rules, and finds problems early. Checking suppliers often keeps the supply chain strong and ready for changes. Good supplier management helps keep quality high and meet the rules’ needs.
Regulatory Submission
Documentation Prep
Getting ready for regulatory submission takes careful planning and organization. At NOBLE, we help teams collect and prepare all required documents to meet global standards like the FDA, European MDR, and ISO 13485.
The process starts with building a technical file. This includes the device design, how it’s made, risk management details, and proof that the device meets safety and performance standards. We help prepare clear Instructions for Use (IFU), check that labels and packaging follow rules, and make sure all files are ready for electronic submission.
Before sending the documents, NOBLE carefully reviews everything for accuracy and quality. We also help write a strong cover letter that summarizes the device and shows proof it works well. After submission, NOBLE stays involved—tracking the review status and helping respond to agency questions. We also support post-market surveillance, like collecting feedback from clinics and reporting any problems.
For devices that include software, NOBLE helps prepare all necessary software documentation, including the Level of Concern statement, hazard analysis, design details, and a traceability matrix.
Approval Process
The approval process for medical devices is different in each place and for each device type. In the United States, the FDA has a few ways to get approval. The 510(k) pathway takes about 3 to 9 months. The De Novo pathway takes about 1 to 1.5 years. The PMA pathway for high-risk devices takes about 1.5 to 2 years. In Europe, the conformity assessment usually takes more than a year because the rules are stricter and there are not many notified bodies.
| Region | Average Approval Time |
| USA (510(k) pathway) | About 3 to 9 months |
| USA (De Novo pathway) | About 1 to 1.5 years |
| USA (PMA pathway) | About 1.5 to 2 years |
| Europe (Conformity Assessment) | Usually over 1 year |
The manufacturer should keep track of the submission status, answer agency questions quickly, and get ready for audits or checks. After approval, companies must keep watching the device and keep up their quality systems.
Post-Market Activities
Surveillance
When a medical device is sold, companies must watch how it works. Post-market surveillance (PMS) helps find problems early and keeps people safe. The United States and Europe both have strict PMS rules. The table below shows how their rules are alike and different:
| Aspect | United States (FDA) | Europe (EU MDR 2017/745) |
| Regulatory Basis | 21 CFR Part 803 (Medical Device Reporting), 21 CFR Part 822 (Post-market Surveillance) | EU Medical Device Regulation (EU MDR 2017/745), Annex III PMS requirements |
| Reporting Timelines | Adverse event reports within 30 days of awareness | Serious incidents are reported within 2, 10, or 15 days, depending on severity |
| PMS Plan Requirements | PMS Plan required upon FDA order; must address specific surveillance questions | Comprehensive PMS Plan required for all devices; holistic lifecycle approach including proactive data collection |
| Data Collection Methods | Investigation of adverse events, root cause analysis | Proactive and systemic data collection, including user feedback, literature, registries, and social media |
| Post-market Clinical Follow-up (PMCF) | Required for certain devices under FDA orders | PMCF Plan mandatory as part of PMS Plan; continuous clinical data collection and evaluation |
| Reporting Obligations | Submission of adverse event reports, supplemental reports if new information arises | Periodic reports such as PMS Reports for Class I, PSURs for Class IIa and above, Summary of Safety and Clinical Performance (SSCP) for higher classes |
| Surveillance Period | Begins within 15 months of FDA order; can last up to 36 months | Continuous throughout the device lifecycle |
| Vigilance Definition | Reporting of adverse events and malfunctions that may cause serious injury or death | Vigilance includes serious incident reporting and is integrated into the PMS system |
| Risk Management Integration | Root cause investigations and corrective actions | Continuous lifecycle risk management integrated with PMS activities |
PMS uses many types of data. We gather info from clinical reports, complaints, event logs, social media, and device lists. We use special tools to look for patterns and make things safer. PMS plans must match the risk class of each device. If we find a problem, we must act fast and fix it.
Continuous Improvement
Continuous improvement is key to keeping medical devices safe, effective, and reliable. At NOBLE, we use Post-Market Clinical Follow-Up (PMCF) to gather real-world data on device performance. PMCF helps us identify new risks, confirm long-term safety, and ensure the device continues to meet user needs. NOBLE works closely with healthcare professionals and regulatory bodies to review data and update devices as needed.
Many companies, including NOBLE, follow Kaizen principles—making small, consistent improvements across all areas. We encourage every team member to contribute ideas to boost quality and reduce waste. Through tools like Gemba walks, quality circles, and visual management, NOBLE actively finds and fixes issues early. These practices lower error rates, improve efficiency, and support reliable production.
Continuous improvement also means staying updated with evolving regulations and adopting new technologies. NOBLE documents every change, evaluates its impact, and ensures updates enhance both safety and performance. This careful tracking builds trust with regulators, users, and partners.
Strong projects follow clear, structured steps from beginning to end. At NOBLE, flexible manufacturing systems, robust risk management, and user training help ensure successful outcomes. Our Quality Management System (QMS) and risk controls are designed to protect patients and support full regulatory compliance. This guide can also serve as a checklist—helping teams avoid mistakes, stay on track, and deliver safe, effective devices to the market.
Many companies use Kaizen ideas to get better. Kaizen means making small changes often. All workers can share ideas to improve quality and cut waste. We use Gemba walks, quality circles, and visual tools to find and fix problems. These steps can lower mistakes and help make more devices.
Continuous improvement also means learning new rules and using new technology. We must write down every change and check if it helps the device. This builds trust with users and rule groups.
- Working with partners and using digital health tools brings new ideas.
- Checking and updating devices often keeps them safe and working well.
Every new Medical device can help people when we care about safety, quality, and always getting better.
FAQ
What is the most important step in medical device development?
All steps are important, but knowing what users need comes first. Those who learn about user needs early make safer devices. This step helps guide choices and stops expensive errors.
How long does it take to develop a medical device?
How long it takes depends on the device type. Simple devices might take one or two years. Harder or riskier devices can take three to seven years. Rules and testing make the process longer.
Why is risk management critical in this process?
Risk management keeps patients and companies safe. We look for dangers, control risks, and write down what we do. This helps stop recalls and makes sure rules like ISO 14971 are followed.
What happens if a device fails post-market surveillance?
If a device fails, the company must check and report the problem. We might recall it, change the instructions, or redesign the device. Rule groups watch these steps to keep people safe.